Insulin Resistance: The Root Cause of Metabolic Disease (that's never talked about)
If you have never been diagnosed with diabetes, pre-diabetes or gestational diabetes, there’s a good chance you’ve never given much thought to your blood sugar. And it’s true that if your metabolism is operating optimally, there’s not much to think about. A strong metabolism works a lot like a thermostat – regardless of what you eat or drink, your body will maintain a perfect blood sugar level between about 60 – 140 milligrams of glucose per deciliter of blood. What many people don’t know is that a diagnoses of diabetes is typically decades in the making. It all starts with something called insulin resistance…
An alarming number of people in the U.S. already have diabetes (~13% of the population) and pre-diabetes (~35% of the population). That means that almost half the population is already at level 5 on the chart above. You don’t get to that point overnight, which begs the question: how many people are at level 2 (insulin resistance) and have no clue!?
Unfortunately there’s not a great laboratory test for insulin resistance. One thing you can do is utilize two of the more common lab tests as a proxy: triglycerides and HDL.
Triglycerides ÷ HDL
> 3 is a strong indicator of insulin resistance
If you want to dive even deeper, there is a test you can ask for called the HOMA-IR (Homeostatic Model Assessment of Insulin Resistance). HOMA-IR is calculated by comparing two tests, fasting glucose levels and fasting insulin levels. Most doctors will test for fasting glucose alone, and if it’s normal the patient will be assumed metabolically healthy. But it’s possible that your fasting glucose is only normal because your body is pumping out extra insulin to combat insulin resistance. This test can help reveal that circumstance.
Fasting Insulin x Fasting Glucose ÷ 405
Less than 1.0 indicates optimal insulin-sensitivity
1 – 1.9 indicates acceptable insulin-sensitivity
2 – 2.9 indicates early insulin resistance
3+ indicates significant insulin resistance
Aside from the above tests, one other option is to wear a continuous glucose monitor (CGM) for a few weeks. Although this will not show insulin resistance, since it is only monitoring glucose, it will give you a good idea of which foods, drinks and activities affect your blood sugar most acutely. This is an especially useful activity if the tests above did, in fact, indicate insulin resistance, or if you have been gaining weight in your mid-section and can’t figure out why (level 4 on the chart above).
There are two CGMs on the market at this time, the Dexcom G6 and the Freestyle Libre. Dexcom’s device is mainly marketed towards people with Type 1 Diabetes, especially those utilizing an insulin pump. But the Freestyle Libre is very easy to get even if you do not have diabetes. You do need a prescription, but I can’t see why a primary care doctor would hesitate to prescribe a device that simply monitors blood sugar. Once you have the prescription you can buy the Libre at any pharmacy. Insurance typically won’t cover a CGM unless you are diabetic and using insulin to control it, but the out of pocket cost is only about $70-100 for a month of monitoring. It’s not something you would need to do forever – a few weeks of monitoring is very eye opening and can help you make long term diet changes. Below are some insights that I derived from just over a week of monitoring recently.
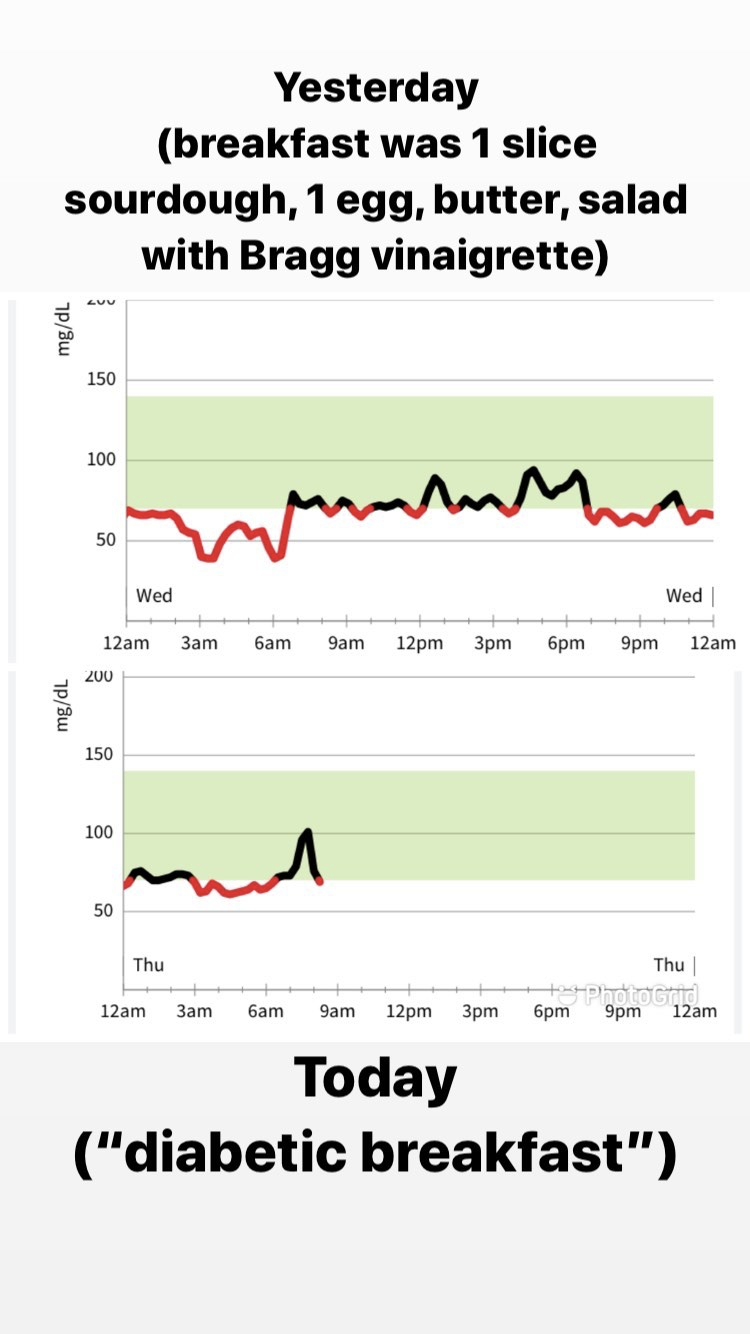
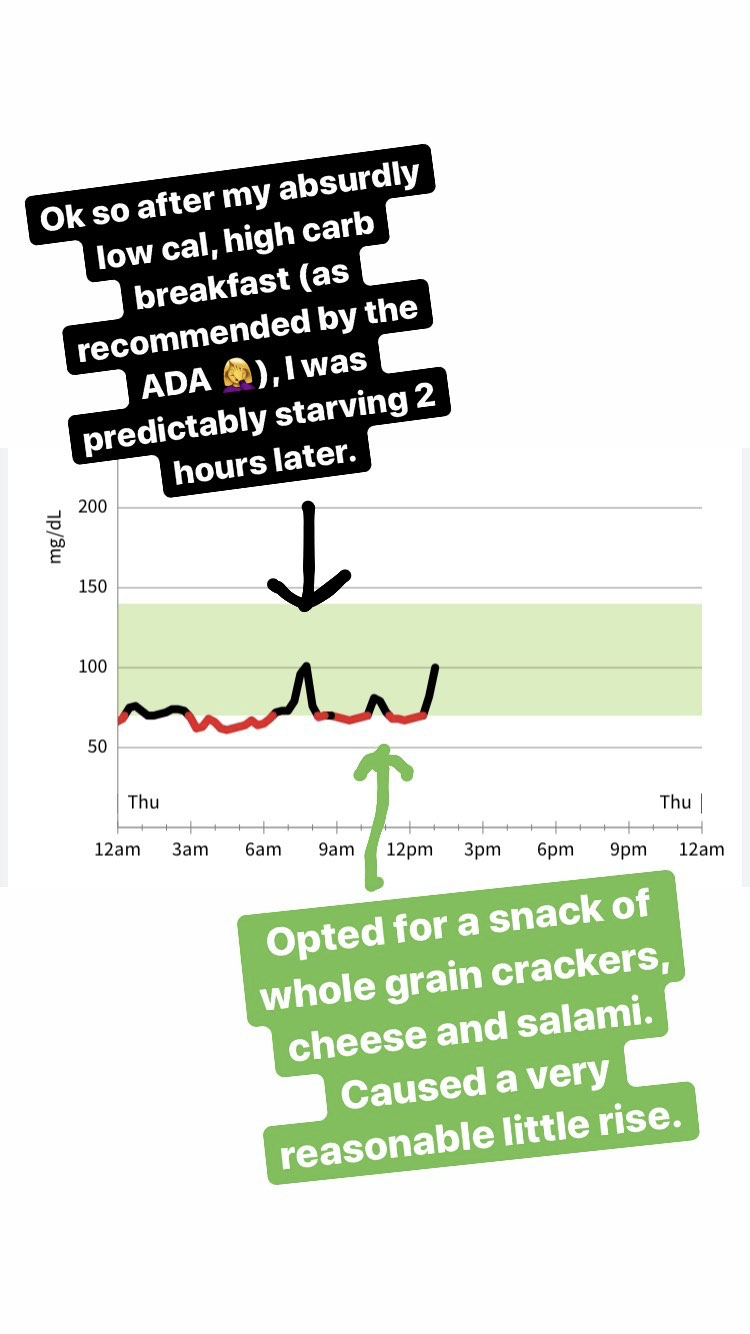
Experiment #1: American Diabetes Association Breakfast
First is a comparison of two different breakfasts. On the first day I ate a breakfast that is fairly typical for me - egg, sourdough bread, butter, veggies. It’s not a low carb breakfast because of the bread, but it’s pretty balanced with plenty of protein and fat. My sugar stayed very stable following that breakfast. On the next day I ate a breakfast that is recommended by the American Diabetes Association: rolled oats cooked with water and topped with a small amount of jelly, blueberries and slivered almonds. My sugar spiked immediately, and then crashed. High carb foods like oats must be paired with ample fat and protein in order to keep sugar stable.
Experiment #2: Fruit as a Snack
Many people choose fruit as a “healthy” snack. But fruit is a high carb, low fat, low protein food. So on this day I wanted to see how my blood sugar would fare if I ate grapes as a mid-morning snack. Sure enough, it spiked, then plummeted. Eating a similar amount of carbs at breakfast and lunch that day did not result in the same spike, thanks to ample fat and protein in the meal.
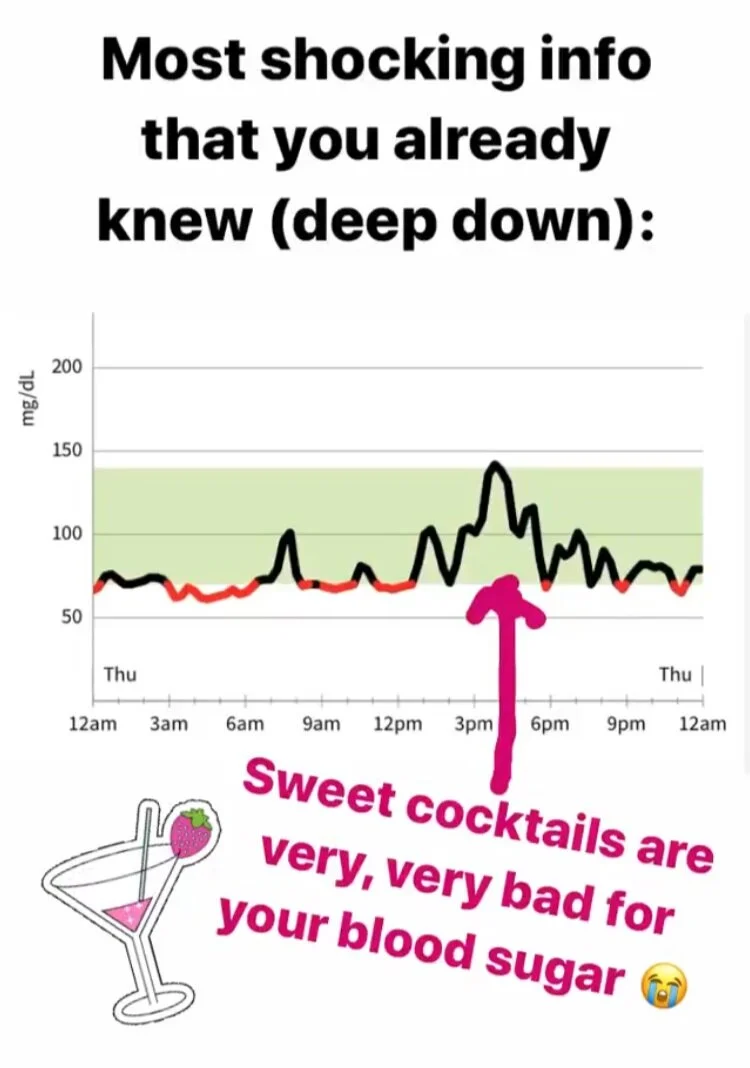
Experiment #3: Sugary Beverages
This is the experiment that everyone can guess the results of. Sugary beverages (in this case sweet cocktails) WILL RAISE YOUR SUGAR. Keep in mind, I am not diabetic. I’m not even pre-diabetic. Any doctor would take one look at my labs and weight and pronounce me healthy. But these drinks sent me squarely out of the “healthy” range (above 140). This means that I am already a little bit insulin resistant. It seems that my body can combat most carbohydrate loads, but it’s no match for liquid sugar.
If you would like to try out a CGM for yourself, I’d encourage you to reach out to your primary care physician about a Freestyle Libre prescription. And if you would like assistance decoding the results, feel free to reach out and we can set up a virtual session.